What is MRSA?
MRSA is the abbreviation for “methicillin-resistant Staphylococcus aureus”. MRSA germs thus count as staphylococci, a widespread group of bacteria. Like other staphylococci, MRSA is often found on the skin and mucous membranes of the upper respiratory tract of humans and animals. What is special about the MRSA germ is that many antibiotics do not have any effect on it – it is multi-resistant.
(c) Freepik
How is MRSA transmitted?
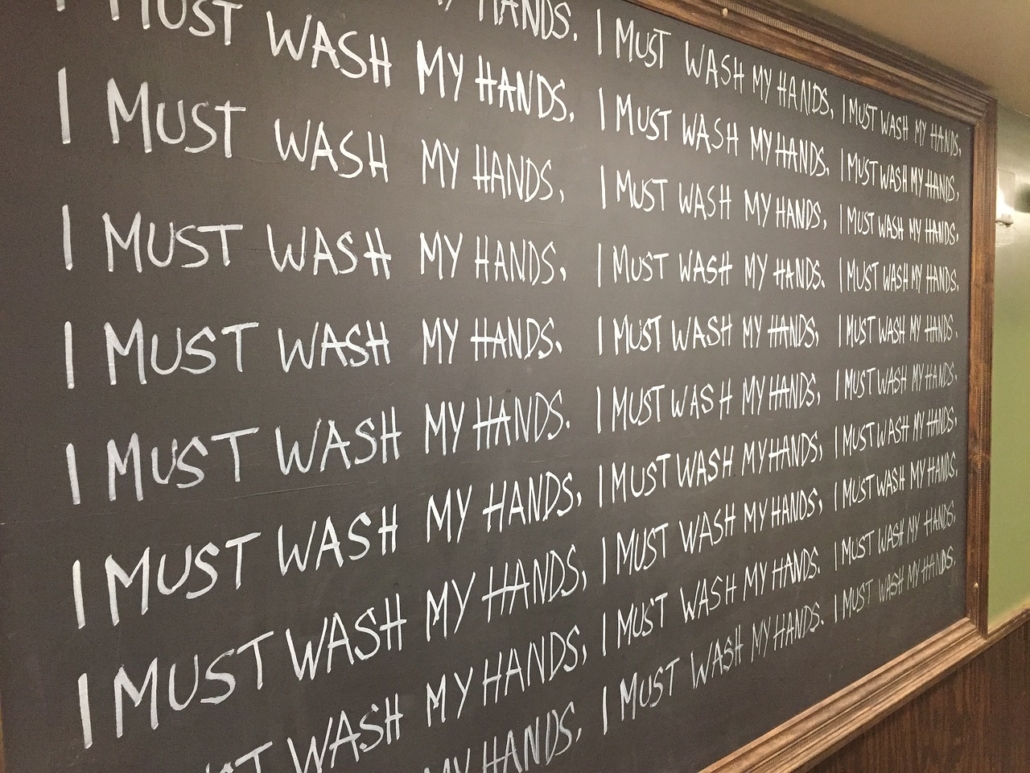
The pathogens are most frequently passed on from person to person by direct contact. The main transmission path are the hands. Both, MRSA patients and MRSA carriers can be vectors. The latter can also infect themselves if, for example, they transfer the bacterium from the nasal atrium into an open wound. Contact with contaminated objects such as door handles, handrails, handles or bathroom utensils may also result in infection. The pathogens adhere very well to plastic materials and stainless-steel alloys, such as catheters.
In recent years, commercial livestock farming has led to the development of a new source of MRSA infection for humans. Infections with LA-MRSA can occur in people who have direct contact with farm animals in mass livestock farming (especially pig and poultry fattening facilities). For example, farmers, veterinarians or slaughterhouse employees are affected.
How can an MRSA infection be detected?
If MRSA penetrates the tissue during an infection, the disease initially proceeds like an infection with “normal” staphylococci, i.e. it also shows the same symptoms: dermatitis (such as ulcers or pus accumulation), wound infections (especially after operations and inflammations of individual organs) such as urinary tract infections, pneumonia or bloodstream infections. Due to the existing antibiotic resistance, however, such MRSA infections (especially in septicaemia) are much more difficult to treat with medication, so that the disease can be life-threatening.
When does the disease break out and how long is a person contagious?
MRSA does not necessarily have to cause a disease. In people who are colonized with MRSA, a disease can break out when the immune system is weakened and the bacteria find their way into the body. The afflicted are contagious as long as the pathogen can be detected.
How long is the incubation period?
Approximately four to ten days after MRSA infection, the first symptoms appear. However, people who are not infected with MRSA, but only colonized, often do not experience any symptoms at all. In some cases, the germs simply live permanently on the skin and mucous membranes without causing harms.
How is an MRSA infection diagnosed?
For the tests, swabs are generally taken from the nasal atrium, pharynx, armpits and groin respectively pus or wound secretion from the infected tissue is collected. The testing also shows which antibiotic resistances are present in the MRSA germ. Such an antibiogram shows which medication is no longer effective against the pathogen and which is the most promising.
How are MRSAinfections treated?
In the case of an MRSA infection, the therapy usually consists of a special combination of different antibiotics. The threating physician selects exactly those antibiotics, that have been shown to be effective against the germ in the laboratory test (antibiogram), such as glycopeptide antibiotics together with rifampicin, clindamycin or gentamicin A combination of fosfomycin and fusidic acid is also possible. Drugs from the group of beta-lactam antibiotics are not suitable for therapy, because MRSA germs are resistant to them.
If the treating physician decides on MRSA therapy with only one single antibiotic, he or she can also resort to the active substance linezolid. Other drugs that can also be used in MRSA are tigecycline, daptomycin or newer cephalosporins.
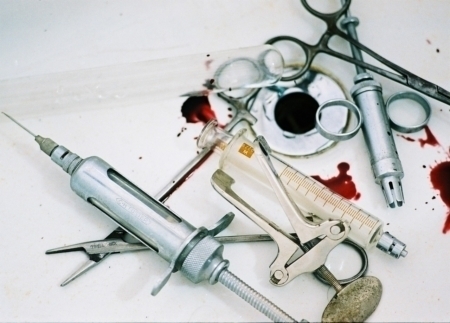
How can MRSA infection be prevented?
Hospitals and care facilities can basically prevent the spread of MRSA easily by strictly adhering to certain hygiene measures: The spread of MRSA bacteria can be reduced by physicians and nurses through disinfecting their hands, disinfecting objects and wearing disposable gloves. Visitors should also use the hand disinfectants provided before and after each visit.
If an MRSA infection has been treated with antibiotics, this does not mean that the affected person is free of MRSA afterwards. As a rule, this is only the case if MRSA has also been remediated. After an MRSA infection has been treated, there is still often a colonisation with MRSA, but there are no symptoms. In this casefamily members or the immediate social environment do not have to worry about contracting MRSA. The risk of infection is very low for healthy people. Nonetheless, kissing or close physical contact can lead to temporary colonisation, which usually passes without symptoms.
However, people with open wounds or skin injuries should take precautions. This also applies to people who are generally susceptible to infections with staphylococci, such as people with chronic diseases (e.g. diabetes) or with a weakened immune system (e.g. after organ transplantation or due to HIV). In such cases, the treated MRSA patient should remain physically separated from others until complete MRSA remediation.
The approach in the Netherlands is partly different from that in other European hospitals. Since the 1980s, the so-called search-and-destroy-strategy has been pursued: every patient who might have MRSA is isolated and swabs are taken. Until it is clarified, the patient is treated in isolation. Swabs must also be taken from all contact patients. Patients or staff who appear to be positive for MRSA are treated with decontamination products. These are nasal ointments and chlorhexidine liquid soap, with which skin and hair have to be washed. If the MRSA bacteria also cause an infection, antibiotics are used. Physicians in the Netherlands are very cautious about employing antibiotics in order to avoid resistances. Due to the active search for MRSA, the screening strategy, and the moderate use of antibiotics, MRSA is relatively rare in the Netherlands compared to other countries.